With COVID-19 disrupting every aspect of life, it’s more important than ever to keep potential outbreaks under control, help economies recover as quickly as possible, support the roll-out of vaccines, and safely end global travel restrictions.
By the end of 2020, over 11.5 million people in the Asia-Pacific region had contracted COVID-19, with an average mortality rate of 1.5%. The pandemic and the stringent restrictions that followed have severely impacted the region’s economies, some of which experienced a GDP contraction of up to 6%. Lately, new variants with potentially greater infectivity have been identified in South Africa, Europe, and Asia, and such mutations are expected to evolve with increasing spread. Testing strategies play a pivotal role in gaining an understanding of the rate of transmission, and in the identification of hotspots with existing or new viral strains for early isolation and response.
As of January 2021, different vaccines have been approved for use, while others are at different stages of clinical trials. Government agencies and vaccine suppliers face ongoing challenges over vaccinating the whole population against a backdrop of limited supply. The long-term efficacy and safety of vaccines (six months after use) are mostly unknowns. It thus becomes critical to monitor for population-scale side effects and effective immunity following vaccine roll-out. Furthermore, assessment of vaccine efficacy in response to emerging new strains needs to be routinely monitored. Finally, the extent to which vaccines will limit disease transmission is still unknown, underlining the continued need for testing to stop transmission.
Thus, alongside therapeutic and preventive measures to tackle COVID-19, a robust testing strategy is crucial for optimal public health outcomes (e.g., case numbers, disease prevalence, vaccine efficacy) and economic outcomes (e.g., economic recovery, reopening of businesses), aspects of which include the early identification of hotspots with asymptomatic cases, rapid isolation to contain the spread of the disease, and the appropriate allocation of resources for preparedness to manage future outbreaks. Implementing asymptomatic screening on a national scale is essential but comes with challenges:
- Limited resources and capabilities to lift testing capacity (supply of diagnostic kits, trained staff).
- Inaccessible testing centers and an over-reliance on a limited number of institutionalized centers like hospitals, that are also perceived as ‘high risk’ venues by patients.
- Long waiting times for sample submission and collection making the process cumbersome for the public.
- A lack of centralized coverage for diagnosis and corresponding treatment costs deterring low-income sections of the population from undergoing testing.
This review highlights use-cases of testing strategies and technologies already being used to confront various pandemic scenarios and challenges. Drawing on global and regional use-cases of testing, this paper evaluates the new imperatives in testing to contain COVID-19 spread and reduce the risk of case resurgence and allow the re-opening of economies.
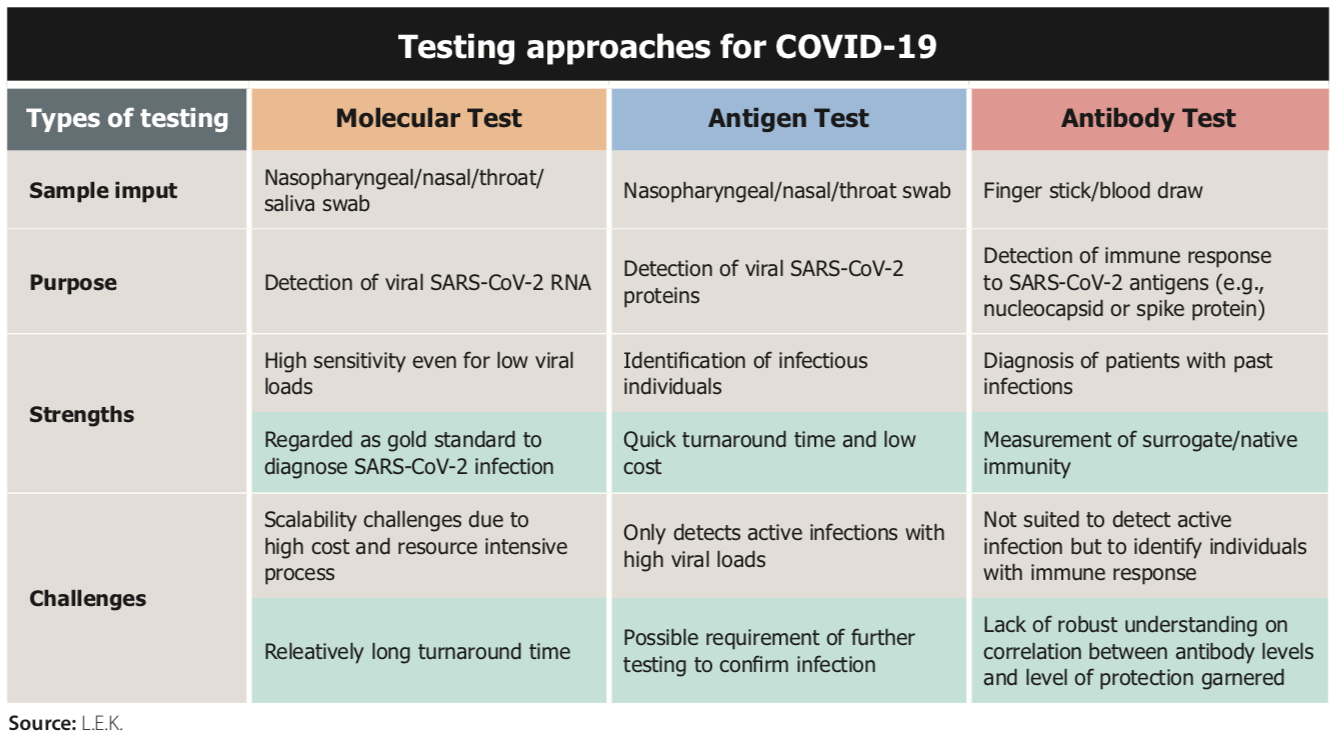
There are three main approaches to COVID-19 testing for both symptomatic and asymptomatic individuals. At the close of 2020, molecular test remains the gold standard diagnostic test, given its highest sensitivity to low viral loads. Antigen testing detects high viral loads and is useful to assess infectivity of an individual typically within the first week from the formation of a detectable viral load. Emerging global guidance suggests that antigen testing can be used to rapidly identify infectious individuals. Since the viral load curve is similar between symptomatic and asymptomatic patients, antigen testing can be utilized to identify infectious patients in both populations within the first 10 days of infectiousness. Frequent antigen testing (every 1-3 days in high exposure areas) can be leveraged to deliver comparable or higher sensitivity to molecular tests. Antigen testing further presents advantages due to the rapid turn-around times and lower skill-set requirements to conduct the test.
Antibody/serological tests, on the other hand, are most sensitive 2-4 weeks after exposure and, as antibodies may persist for months thereafter, the test is useful to aid diagnosis of patients who present late after symptom onset, and to perform epidemiological surveillance. Antibody tests may indicate the presence of protective immunity against SARS-CoV-2, although this awaits further evidence. Proactive screening for antibodies can also be used to identify plasma donors for convalescent plasma therapy, which is being actively researched for therapeutic use in India, and the US.
Summary of recommendations
There exists a spectrum of practices that have already been widely adopted in select countries and those that continue to emerge in others. Summarized below are a set of recommendations for integration of robust testing strategies across different scenarios in COVID-19 management.
Future pandemic preparedness
The healthcare and economic challenges posed by COVID-19 throughout the world are unique in the last century. Through the extraordinary commitment of health officials, providers, HCPs and their partners in industry throughout the last year, the APAC region already has access to a wide array of screening and other diagnostic tools and techniques that can help manage the pandemic and limit its negative effects on society. This review has shown the utility of these new tools in practice in the region, and we encourage all stakeholders to fully leverage this ‘toolset’ to return societies as fast as possible towards economic growth and reopening.
A combination approach of diagnostics based on context/nuance of the specific situation is deemed important for consideration in the management of COVID-19. Another element for consideration would be leveraging standardized, interoperable digital platforms supplemented with privacy regulations to establish proof of testing and/or vaccination. The recent guidelines on proof of vaccination for medical purposes by the European Commission highlights the need to have such an initiative in place.
Future outbreaks, though inevitable, can be contained early with appropriate preparedness measures in place. This includes collaborations at regional and global levels to ensure harmonization of public policies for testing strategies and response. Such measures can be further supplemented with open public communication of up-to-date information on testing strategies and guidelines to align all the stakeholders involved. Considering the challenges encountered in this pandemic, countries are already taking steps to conduct epidemiological surveillance to look out for high-risk viral strains that might be the cause of the next outbreak or surge. It is further essential that such surveillance data is shared at a regional level to closely monitor any developments and initiate response to minimize both health and economic impact.
This report was produced by APACmed and L.E.K. A full copy of the report can be downloaded at the AmCham China Travel & Vaccine portal here.
This article is featured in our Quarterly Magazine. Access the full issue in the Publications tab after logging into our member portal here.

